SmartDerm: Using Technology to Prevent Bedsores
Hanmin Lee, MD, surgeon in chief of UCSF Benioff Children’s Hospital San Francisco and director of the UCSF Fetal Treatment Center, has pioneered many treatments for rare conditions in fetal and pediatric patients.
Now, one of his latest projects seeks to prevent a very common condition: pressure ulcers, also known as bedsores, which can develop in as little as two hours when constant pressure on the skin reduces blood flow and causes tissue death.
“I’ve seen pressure ulcers start in the operating room during long operations, and six years ago, I thought, ‘This is an obvious thing to focus on,’” said Lee. “Interestingly, most other people said, ‘Why would you work on such a mundane problem?’ But today, everybody is interested.”
Economic forces drive much of that surge in interest: in 2006, Medicare regulations changed to discontinue reimbursement to hospitals for care of several preventable conditions, including pressure ulcers.
To address this complex problem, Lee brought together a multidisciplinary team, including bioengineers Sachin Rangarajan, MTM, and Michael Hemati, MTM – both graduates of the joint UCSF-UC Berkeley Master in Translational Medicine Program – and surgical resident Isabelle Chumfong , MD, MEng. Together they are developing SmartDerm, a wearable sensor which continuously measures pressure levels on the skin.
Nurses currently try to prevent pressure ulcers by turning patients frequently, but this approach is labor-intensive and not always successful. “All our [previous] solutions have been to add more people, more time, more eyes … but there’s probably a way to intervene in a smarter way that doesn’t utilize all these resources,” said Chumfong.
How It Works
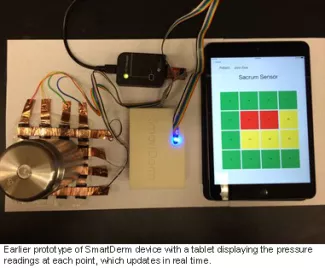
Nurses currently place wound dressings on high-risk areas, such as the lower back, to slow the development of pressure ulcers. The SmartDerm team embedded these dressings with a paper-thin grid of sensors that detects pressure at 16 different points. The sensors connect with a postage stamp-sized Bluetooth device which wirelessly feeds continuous pressure readings into a computer. A tablet displays pressure readings at each of the 16 points, colored green, yellow and red for low, medium and high pressure levels – which update in real time, as a patient moves or is turned.
The current design is a result of many refinements. The early prototypes that Rangarajan and his colleagues developed for his master’s program project had a lot of blinking lights and protruding wires. “The other students kept calling it the ‘torture device,’” said Rangarajan. “They said, ‘Why is this device angry? Why is it blinking at me?’ As an engineer, the more information we’re getting from the device, the more comfortable I feel.” Thanks to this early-stage feedback from peers, Rangarajan was able to develop a more streamlined version that was less likely to contribute to alarm fatigue, and would only display the most essential information needed by clinicians.
Chumfong helped propel another critical stage of the process. Inspired by her recent externship at design firm IDEO, she recognized the importance of involving frontline users in the design process, and arranged for Rangarajan and Hemati to gather feedback from nurses and patient care assistants.
Rangarajan and Hemati thought the nurses would want transparent sensors so they could visually monitor the skin. However, they learned that nurses only needed to see the skin when changing the dressings every few days. That simplified one aspect of the process, since the team could embed the SmartDerm sensor in opaque, off-the-shelf wound dressings rather than invent new transparent dressings from scratch. It also increased the nurses’ willingness to use the device. “When they saw the form factor of a wound dressing that they’d already used and were comfortable with, they were a lot happier,” said Rangarajan.
The Pressure is On

One next step is to develop a better understanding of what constitutes low, medium and high pressure for specific patient populations. Interestingly, even though pressure ulcers affect about 2.5 million Americans annually and cost an estimated $11 billion, there is very little research about how much pressure actually causes a bedsore.
Although nurses and doctors had a general sense of conditions that predispose patients to developing pressure ulcers, the team used a big data approach to develop a more statistically robust list of risk factors. They analyzed database records of millions of hospitalized patients, finding that advanced age, diabetes, pre-existing skin conditions, poor circulation and sepsis were among the conditions associated with bedsores. They are now analyzing records from UCSF patients who did and did not develop pressure ulcers, using a machine learning approach to identify clusters of patients who are at higher risk of developing bedsores.
The SmartDerm team is has recently begun observational studies, initially using the sensor to collect pressure information from patients in the UCSF neuro-intensive care units (ICUs). “The neuro-ICU nurses are really great at adopting new technologies and giving feedback, so we’re starting there to test it out, make a few more refinements, and then expanding out,” said Rangarajan. The team will eventually collect continuous pressure information from patients at UC Davis, UC Irvine, UCLA and UC San Diego.
The team will use machine learning algorithms to identify patterns in pressure changes preceding the development of a pressure ulcer. While continuous pressure buildup can lead to a pressure ulcer, studies have demonstrated that cycles of ischemia and reperfusion – inadequate blood flow followed by restoration of blood flow – are an important mechanism in the development of pressure ulcers. Also, certain repeated compression and release cycles can lead to even greater tissue injury compared with constant pressure over the same period of time. This highlights the complicated nature of pressure ulcer formation and underlies the usefulness of the machine learning approach. “We don’t know what exactly leads to these pressure ulcers, but with our device we can exactly see the change in a patient’s pressure profile before the ulcer occurs, and with enough data, machine learning will enable us to identify the specific patterns in pressure profile changes that correlate with ulcer formation,” said Rangarajan.
Prevent and Improve
Eventually, the SmartDerm group hopes their device can help prevent bedsores from forming. “We can help a nurse triage whichever patients are at highest risk of developing pressure ulcers,” said Chumfong. “In the same way a pulse oximeter can serve as an early warning system to let us know if a patient’s oxygenation is poor, we want our pressure sensors to let providers know when a patient’s exposure is risky so they can intervene.”
One of the advantages of SmartDerm is that the sensor is active whether the patient is lying in bed, in another part of the hospital undergoing tests, or sitting in a chair – which can also contribute to the development of bedsores.
The group also hopes to eventually improve existing technologies, such as air mattresses that continuously reposition patients. “Patients dislike air mattresses because they can be noisy and uncomfortable,” said Rangarajan. “Another device places the patient in a sling-like device, which is used to lift and drop the patient into a new position with overly exaggerated movements. We likely could partner with existing bed technologies or even develop a more localized repositioning tool, since we think by knowing the real-time pressure, we would only need small adjustments rather than these exaggerated movements to relieve pressure buildup.”
The SmartDerm team hopes their device will eventually interface with electronic medical record systems, automatically notating when patients are turned so nurses can spend less time documenting their work and more time directly caring for patients.
Bringing Innovation to Patients
In addition to the design, engineering and clinical trial aspects, the SmartDerm team has also been focused on marketing, pricing and gaining regulatory approval from the US Food and Drug Administration (FDA). “We’ve talked to hospital value analysis committees and learned about the complex decision-making process involved in purchasing and reimbursing new medical devices,” said Rangarajan. The group has also compared the FDA approval process with regulatory processes abroad, and worked with a team of business students from the University of Strathclyde in Glasgow, Scotland to develop an internationalization plan. “Working on SmartDerm has given me exposure to a variety of fields and skills beyond engineering that are involved in innovating medical devices and it’s been a great learning experience – closer to a startup than a pure academic experience,” he said.
“UCSF has incredibly high levels of talent and collaboration, as well as a strong ethos for really wanting to help people,” said Lee. “We want to push forward research so that products get to patients. When you can see how the field is evolving, you’ve got a head start. Wayne Gretzky’s dad said it the best: ‘Don’t skate to where the puck is, skate to where the puck is going to be.’”
by Elizabeth Chur
