Georg Wieselthaler: "Stay hungry. Stay foolish"
This profile was originally published on the UCSF Division of Cardiology website. It is reproduced here with permission.
"Stay hungry. Stay foolish."
Dr. Georg Wieselthaler (pronounced “VEE-zell-tall-ah”), UCSF’s director and surgical chief of Cardiac Transplantation and Mechanical Circulatory Support, said that these words from Steve Jobs’s 2005 commencement speech at Stanford University are the wisest he has ever heard.
“You have to be a little bit foolish to think beyond the rim of your teacup,” said Dr. Wieselthaler, who was recruited from the Medical University of Vienna in Austria in November 2011. “If you walk on a path that 100 other people have walked in front of you, without looking to the left or the right, you’ll never find something outstanding. But if you’re a little bit crazy, you get new ideas, and sometimes it really works out.”

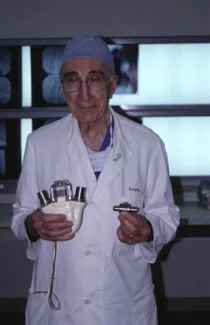
Dr. Wieselthaler’s own career is proof of this belief. A renowned heart transplant surgeon and leading expert in heart pumps which provide mechanical circulatory support for end-stage heart failure patients, in 1998 he implanted a new miniaturized pump into the world’s first long-term survivors. In 2006, he was the first to implant the HeartWare HVAD, another small pump which offers heart failure patients facing certain death a bridge to transplant until a suitable donor organ can be found. Dr. Wieselthaler also trained as an electrical engineer, and this expertise has allowed him to develop and refine many other pumps.
At UCSF, Dr. Wieselthaler’s first goal is to relaunch the heart transplant program, which had been put on hold after Dr. Charles Hoopes departed for the University of Kentucky. Dr. Wieselthaler and the heart transplant team successfully performed their first heart transplant in March. “We have to prove once again that we can not only technically perform heart transplants, but also produce excellent outcomes,” said Dr. Wieselthaler, who has performed or supervised 400 heart transplants and implanted about 250 mechanical assist devices so far in his career. “We owe this to our patients and referring cardiologists. I also have the intention to ramp up our program.”
Dr. Wieselthaler also wants to bring the latest innovations in mechanical assist devices to patients, and to make discoveries about how to further improve these pumps. “We are at a turning point,” he said. “The old-fashioned devices tried to mimic the pulsatility of the heart, but they have more or less been replaced by the new generation devices, which provide continuous flow. Although they do not mimic the natural heart, they are as effective as the old pumps, and are much smaller. The battery and driving units are getting smaller, so the quality of life of these patients is tremendously improved. It’s a new era in the treatment of these patients.”
Engineering and Medicine

Dr. Wieselthaler grew up in a village in southern Austria, where he developed an interest in medicine and surgery from assisting his father, a veterinarian. In addition to caring for cats and dogs, they occasionally treated more unusual species. Dr. Wieselthaler remembered one client who ran a snake farm, breeding boa constrictors, cobras and crocodiles. One day, the man’s employees brought over a large wooden box containing a five-meter-long python. The snake had gotten into a fight with another python, sustaining numerous deep cuts from the other python’s razor-sharp teeth.
“We put the snake to sleep, and my older brother, my father and I made about 340 stitches,” said Dr. Wieselthaler. “The good part was, we didn’t have to take out the stitches, because as soon as the snake shed its skin, the stitches went along with it.”
Although he had this early exposure to medicine, Dr. Wieselthaler decided to become an electrical engineer. After earning his degree and starting a job at a power supply company, however, he found the work less interesting than he had hoped. Around that time, his mother was in a car accident, and died from a brain hemorrhage. “I realized the doctors were so helpless,” recalled Dr. Wieselthaler. “They said, ‘She has a hemorrhage, and there is nothing we can do.’ I said, ‘That can’t be true. There are lots of smart people in the field,’ and decided to become a doctor.”
His father supported him through medical school at the Medical University of Vienna. “I’m really grateful that my father gave me that kind of opportunity, because I love my job – I love to work with patients, and I’ve been very dedicated to them, all my life,” said Dr. Wieselthaler.
During medical school, a fellow student told him about a job opening taking care of calves which were receiving newly developed heart pumps developed by the university’s bioengineering department. “I immediately fell in love with what I was doing,” said Dr. Wieselthaler. Soon the faculty realized that he also had an engineering background, and persuaded him to work in the bioengineering lab, developing the driving unit for a total artificial heart. He later had the opportunity to observe the first implants of this device in humans, end-stage heart failure patients who were near death and had no other hope.
“The operation was very traumatic to the patient, because you cut out the natural heart, implanted these two artificial pumps in their chest, and had these big thick driving tubes coming out of the body,” said Dr. Wieselthaler. “My friend, who was also a bioengineer by profession, and I watched all this blood dripping, and said, ‘Oh, my God, this is not the way it should be. It should be smaller and easier.’ That was when we started thinking about it.”
A New Type of Pump
He and that friend, Dr. Heinrich Schima, went on to become lifelong collaborators in the pursuit of developing better heart pumps. At the time, the conventional wisdom was that such pumps needed to mimic the pulsatility of the natural heart. The design problem is that so far, no one has been able to develop a device that is as small, efficient and elegant as the human heart. Pulsatile pumps remain large, unwieldy and difficult to implant.
Drs. Wieselthaler and Schima decided to buck the trend and work on developing a nonpulsatile pump – one with continuous flow powered by a small propeller-type motor. At this time, there were only a few other groups worldwide that were working on such an approach. In the late 1980s, before the Internet, it was difficult to rapidly share emerging knowledge.

Drs. Wieselthaler and Schima decided to convene a meeting. “We wanted to bring the specialists together in a place where they couldn’t escape, where they had no chance to go off sightseeing or shopping,” said Dr. Wieselthaler with a smile. So they booked a ski resort near Salzburg in early December 1988, before ski season began. Between 70 and 80 world experts attended the three-day workshop, and the group was snowed in under about 15 feet of snow.
“This was a really seminal meeting to all of us,” said Dr. Wieselthaler. “If you can’t go outside, you have to stay inside and make yourself comfortable. We were all sitting around the fireplace with a glass of wine in our hands, warming up and discussing problems you could face with nonpulsatile flow. It was very fruitful, because we had a lot of good response within a very short period of time.”
The meeting was so successful that the group repeated the experience in 1991 in another isolated location close to Vienna. A year later, a number of the attendees founded the International Society of Rotary Blood Pumps; Dr. Wieselthaler was recently elected to serve as the group’s president.
One of the attendees at the first meeting was Dr. George Noon, a close associate of legendary cardiac surgeon Dr. Michael DeBakey at Baylor College of Medicine. In part through this connection, Dr. DeBakey eventually chose Vienna as one of two centers where the new MicroMed DeBakey Ventricular Assist Device was first implanted in humans. This was the first time that nonpulsatile technology was ever tried in humans for long-term support. The device supports the left ventricle, the powerhouse chamber of the heart which pumps oxygenated blood to the entire body.
Dr. Wieselthaler had been chosen by his department chair to lead the partnership with Dr. DeBakey in Vienna. Dr. Wieselthaler screened many patients, and in the fall of 1998, found two men with end-stage heart failure who were appropriate candidates for the procedure.
The very first devices were implanted in two patients at the German Heart Center in Berlin, but unfortunately both patients died soon after the procedure. However, four days later, Dr. DeBakey’s team came to Vienna, and Dr. Wieselthaler successfully implanted the two patients he had identified. Both men survived and subsequently received heart transplants. One of the patients died a year later of cancer, but the other patient is still alive and well. Dr. Wieselthaler has since implanted more than 80 patients with this device.
Pioneer in Research
In addition to performing these groundbreaking procedures, Dr. Wieselthaler has been a leader in research. In the 1990s, he and his collaborator, Dr. Schima, developed the “Viennese Centrifugal Pump,” one of the first miniaturized prototype devices to use a magnetically levitated bearing at the inflow of the pump. Other pumps at the time used standard mechanical bearings, similar to the tip of a ballpoint pen. These mechanical bearings held the rotor in position, but eventually wore out due to the continual friction. The magnetic bearing employed by Drs. Wieselthaler and Schima eliminated mechanical wear and tear, pointing the way to devices that could last for years.
(Unfortunately, funding for their lab ran out, putting the brakes on their research. However, this magnetically levitated rotor technology is used today by devices such as the HeartWare HVAD™ Pump, an investigational device currently under study in the United States. In the mid-2000s, Dr. Wieselthaler served as a consultant on the development of this device, and also as principal investigator in a clinical trial of the pump.)
Dr. Wieselthaler has also studied the long-term outcomes of patients who received various nonpulsatile devices, including their ability to exercise and their hormone levels after receiving the implants. “There are still a lot of people in the field who say, we need pulsatility – the human race is used to pulsatility over millions of years,” he said. “Now we know these patients can live with these devices over seven or eight years, but there is still a lot of information we are missing. This is one of the goals we have over the next couple of years. UCSF is a good place to conduct this research, because we have excellent researchers here.”
Besides to serving as a bridge to transplant – helping heart failure patients survive long enough for an appropriate donor heart to become available – Dr. Wieselthaler also discovered that implantable mechanical assist devices like the MicroMed DeBakey pump could actually improve the condition of patients who would not be good candidates for heart transplantation.
Some patients with advanced heart failure develop secondary pulmonary hypertension – a condition in which the blood vessels in the lungs constrict and create high pressures and high resistance in the lungs, in response to the impaired pumping ability of the failing left heart. These patients have poor outcomes after heart transplant, and their only hope is to receive a combined heart-lung transplant, which generally has less favorable outcomes than receiving a heart transplant alone. Due to the shortage of donor organs, it also is much more difficult to find two organs for a single patient than it is to find just a donor heart.
Dr. Wieselthaler noticed that patients with high pulmonary pressure who received a pump soon experienced normalized pulmonary pressure, and therefore became viable candidates for heart transplant. Combing through the literature, he found only three papers that anecdotally mentioned this phenomenon. So he and his colleagues conducted a clinical trial of 35 patients, measuring pulmonary pressure before implantation and for several months afterwards; in every patient, pulmonary pressure decreased to a normal level after receiving the pump. “As soon as you resolve the congestion on the left side [of the heart], with the implanted pump, the lung doesn’t see any reason why it should continue to constrict inflow [of blood] – it just releases it,” said Dr. Wieselthaler. “That brings them back to normal vascular resistance, and normal pulmonary pressures. With the pump, we were able to make non-transplant candidates good transplant candidates in a very short period of time.”
Collaborative Discovery
Dr. Wieselthaler is passionate about pursuing research that will improve mechanical assist devices of the future. “We’re still at the very beginning of an evolution, and there is lots of space for research and science,” he said. Building on UCSF’s tradition of interdisciplinary research and his own wide-ranging interests, Dr. Wieselthaler plans to collaborate with cardiologists, hematologists, nephrologists, and many other specialists in conducting research to develop better implantable pumps.
In the spirit of the ski resort meetings which he organized to advance the field of nonpulsatile pumps, Dr. Wieselthaler also co-founded an organization in Austria called the Society for Implantology and Tissue-Integrated Prosthetics. He brought together experts from disparate fields, including a materials engineer who was developing artificial hips, a craniofacial surgeon who implanted artificial jaws, a nanotechnologist, and even a geologist who was in charge of one of the world’s largest meteorite collections and was an expert in metal structures.
“We met every month or so for a good dinner, talking until two or three o’clock in the morning,” he said. “We would relax and think about crazy ideas.” This eclectic group brainstormed out-of-the-box ideas, such as applications of a pump that could be powered by the specific frequency of a sound wave, or the possibility of using nanotechnology to change the surface properties of implant materials such as titanium, a concept that could ultimately eliminate the need for implant recipients to take anticoagulants.
Once the clinical side of the Cardiac Transplantation and Mechanical Circulatory Support Program is solidly re-established, Dr. Wieselthaler is excited to foster interdisciplinary research with colleagues at UCSF as well as throughout the Bay Area and Silicon Valley.
For example, bioengineers have worked hard to develop pumps that do not destroy red blood cells, but they still have a tendency to interfere with platelets or other blood components, which in some cases can cause patients to bleed or, conversely, to form clots. “We still do not have a clue what makes some patients bleed, and others not,” said Dr. Wieselthaler. “There are a lot of things we don’t know yet. We have to investigate.”
Another big challenge is that the current mechanical assist devices have cables that connect the pump with a power source outside the body, exiting the skin and putting the patient at increased risk of infection. Bioengineers are working on a transcutaneous energy transmission (TET) system, in which a coil outside the body transmits energy through the skin to a coil inside the body. Similar to a laptop computer, a buffer battery inside the body provides backup power, allowing patients to detach themselves from the external power source for a few hours to go for a swim or take a shower without having to cover their external cables and battery in a dry bag – activities which are not possible with the current technology. Patients will then be able to reattach their external power source, recharging the internal battery and powering the pump.
New Hope for Patients
Dr. Wieselthaler sees mechanical assist devices as the wave of the future. Because of the overall scarcity of donor organs, the number of heart transplants will probably always be relatively limited. However, many more patients could potentially be helped with a mechanical assist device. Since he arrived at UCSF, Dr. Wieselthaler has been doing outreach to referring cardiologists to highlight some of the latest advances. “There are a lot of patients in the field with end-stage heart failure who could derive long-term benefit from a heart transplant or a mechanical assist device, but they sometimes die before this is taken into consideration,” said Dr. Wieselthaler.
Today, mechanical assist devices are currently approved by the Food and Drug Administration not only for use as a bridge to transplant, but also as long-term, chronic support (also known as “destination therapy”) for patients who are not good candidates for heart transplant because of their advanced age, history of a tumor, or other reasons.
For the right patients at the right time, mechanical assist devices can offer a second chance at life. “Patients with end-stage heart failure can hardly breathe – they fight for every breath,” said Dr. Wieselthaler. “Some cannot leave the house, because they cannot walk. Not all patients can be saved, but there is a large proportion where you can really succeed, even if it’s just for a couple of years. Sometimes it is enough to settle the family affairs, and do things they really want to do. While they are on the pump, they have excellent quality of life – they can fly on planes, go on holidays with their families, play golf. A year to a patient like that, who has been suffering for such a long time, is a gift.”
As he looks forward to expanding the Cardiac Transplantation and Mechanical Circulatory Support Program at UCSF and catalyzing interdisciplinary research, Dr. Wieselthaler looks forward to collaborating with colleagues in all areas.
“I see everything as a team effort,” said Dr. Wieselthaler. “I am not a stand-alone icon, doing things by myself – it’s not possible. For sure, you need somebody to give direction and say, this is our goal. But there are a lot of ways that lead to Rome. … One lesson that I took from my former chief, Professor Ernst Wolner [at the Medical University of Vienna] was… you have to hire the right people and let them work and sometimes get out of their way. Wolner let us young fellows grow and develop, and I want to pass this on.”
This team includes Dr. Ghannam Al-Dossari – another cardiothoracic surgeon who joined UCSF in March – the heart failure cardiologists, residents, nurses, social workers and other professionals at UCSF, and referring cardiologists in the community.
“The vision is to make UCSF an internationally renowned center for end-stage heart failure treatment,” said Dr. Wieselthaler. “It’s all for the benefit of the patients, who are our main interest and concern. We want to give them the best treatment possible.”
- Elizabeth Chur
Photos courtesy of Dr. Wieselthaler
